Tested Positive for GBS? The Specific Probiotic Routine That Might Help
Hearing the words “you tested positive for Group B Strep” can send a wave of anxiety through any expectant parent. Your mind might race with questions and worries about your baby’s safety. Please, take a deep breath. A positive GBS test is not a reflection of your health or hygiene, and it is incredibly common—affecting up to 30% of healthy pregnant people. You have done nothing wrong. This diagnosis is simply a piece of information that allows you and your care team to create the safest possible birth plan for your little one.
While the standard medical recommendation of IV antibiotics during labor is highly effective, many parents wonder if there’s anything proactive they can do beforehand. You might be asking, “Can I change my GBS status? Are there natural ways to support my body?” This is where the conversation about probiotics comes in. This article will walk you through what GBS is, explain the gold-standard medical approach, and then dive deep into the emerging science behind specific probiotic routines that may help support a healthy balance of bacteria, empowering you with knowledge and options to discuss with your provider.
Understanding Your GBS-Positive Result: What Does It Really Mean?
What is Group B Strep (GBS)?
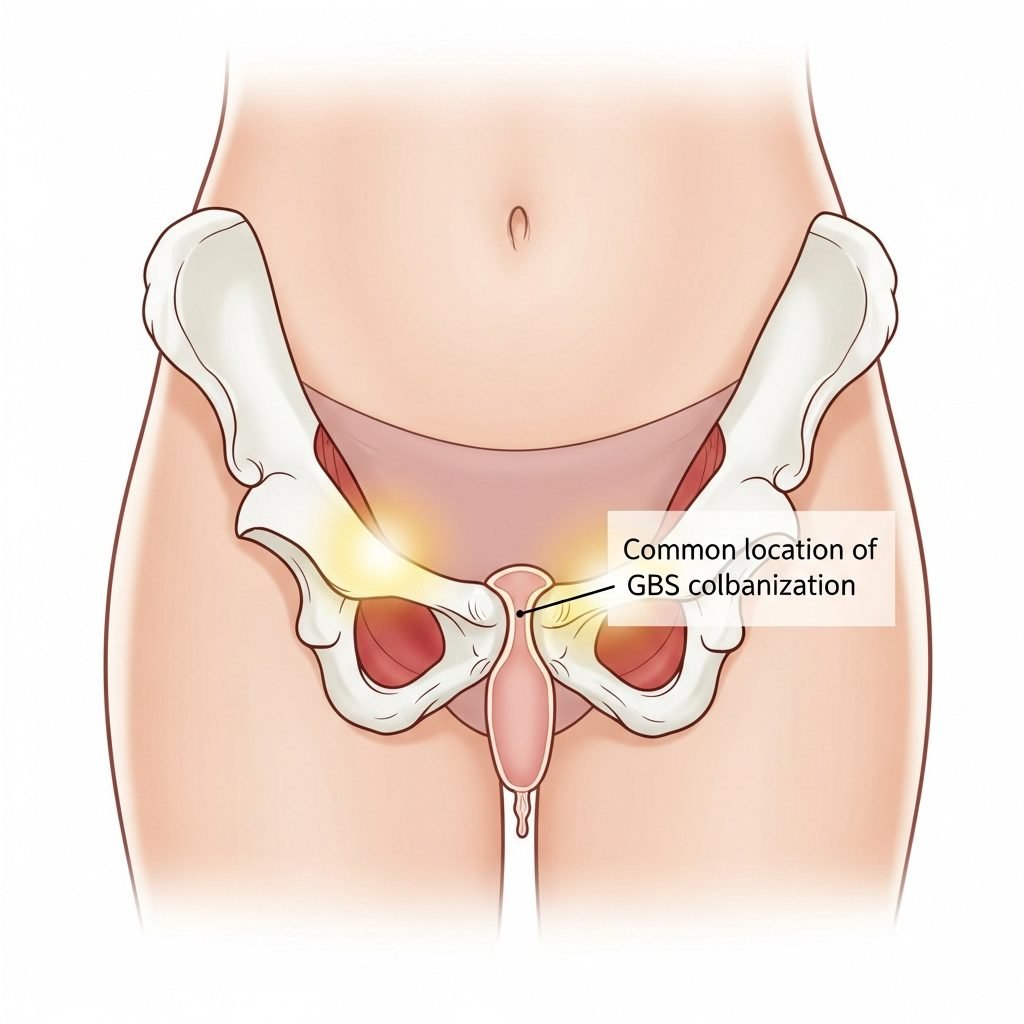
First, let’s demystify Group B Streptococcus. GBS is a type of bacteria that naturally lives in the intestinal and genital tracts of about 1 in 4 healthy adults. It’s important to understand that being a ‘carrier’ of GBS, or being ‘colonized,’ is not the same as having an infection. For most people, it causes no symptoms or harm whatsoever. It can come and go from your body without you ever knowing it’s there.
So, why is it a concern during pregnancy? The primary issue isn’t for the birthing parent but for the newborn. During a vaginal birth, there is a possibility that the baby can be exposed to the bacteria. While the vast majority of babies exposed will be perfectly fine, a very small number can develop a serious illness called early-onset GBS disease. This is why we screen for it between 36 and 38 weeks of pregnancy—knowledge is power, and knowing your status allows your team to take preventative steps.
Key Points to Remember:
- It’s Common: Testing positive does not mean you are unwell or unclean. It is a normal variation of the human microbiome.
- It’s Not an STI: GBS is not a sexually transmitted infection.
- It’s About Prevention: The entire goal of GBS screening and treatment is to prevent a rare but serious infection in your newborn.
Remember, your body is a complex and amazing ecosystem. GBS is just one of many residents. Your positive test is simply an invitation to be proactive for your baby’s health.
The Standard of Care: IV Antibiotics During Labor

When you arrive at the hospital in labor, your GBS-positive status will be a key piece of information for your care team. The universally recommended protocol from organizations like the American College of Obstetricians and Gynecologists (ACOG) is to administer intravenous (IV) antibiotics, typically penicillin, once labor begins or your water breaks. This is usually given every four hours until you deliver.
The reason this is the gold standard is simple: it works. Studies have shown that this single intervention reduces the rate of early-onset GBS disease in newborns by over 80%. The antibiotics don’t necessarily clear the GBS from your system, but they effectively travel through the placenta and into the baby’s bloodstream, providing a protective shield during their journey through the birth canal.
Common Questions About IV Antibiotics:
- What if I have a penicillin allergy? Your doctor will have a plan for an alternative antibiotic, like clindamycin or vancomycin.
- Will the antibiotics affect my baby’s microbiome? This is a valid and important question. Yes, antibiotics can impact both your and your baby’s gut flora. However, the medical consensus is that the proven, life-saving benefit of preventing a potentially devastating GBS infection far outweighs the temporary disruption to the microbiome, which can be supported and rebuilt postpartum through breastfeeding and, potentially, probiotics.
- Do I need antibiotics if I’m having a planned C-section? Generally, if you are having a scheduled cesarean birth before your water breaks and labor begins, IV antibiotics for GBS are not required, as the baby does not pass through the birth canal. However, your doctor will still give you antibiotics to prevent surgical-site infection.
Viewing the IV as a tool of protection, rather than an unwanted intervention, can help shift the mindset. It’s a powerful way you are actively protecting your baby at a critical moment.
The Emerging Role of Probiotics: Can They Help Shift the Balance?
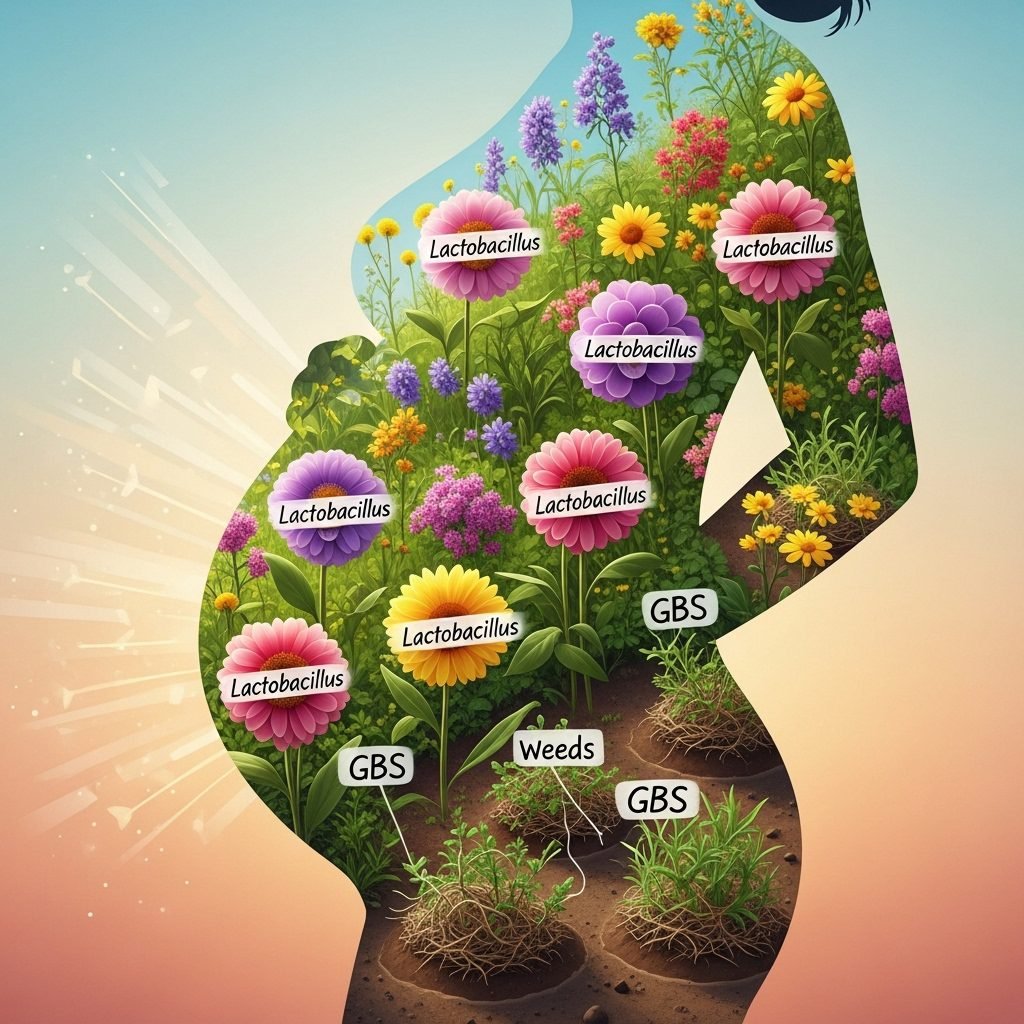
With a solid understanding of the standard medical approach, let’s explore the area you’re likely most curious about: probiotics. The human body, and specifically the vaginal canal, is home to a complex ecosystem of microorganisms known as the microbiome. A healthy, resilient vaginal microbiome is typically dominated by beneficial bacteria from the Lactobacillus family. These good bacteria produce lactic acid, creating an acidic environment that makes it difficult for opportunistic bacteria like GBS to overgrow.
The theory behind using probiotics for GBS is that by introducing specific, beneficial strains of bacteria, you can help bolster your body’s natural defenses and create an environment less hospitable to GBS. The goal isn’t necessarily to completely eradicate GBS—which may not be realistic—but to reduce the overall colonization level, potentially tipping the scales in favor of a negative test result at your next screening or simply supporting overall vaginal health.
It is absolutely crucial to understand that probiotics are not a replacement for IV antibiotics during labor if you are GBS-positive. They should be viewed as a supportive, complementary strategy to be used during pregnancy under the guidance of your healthcare provider.
Research in this area is promising but still evolving. Several clinical studies have investigated the effects of specific probiotic strains on GBS colonization, with some showing a significant reduction in GBS-positive rates among participants who took oral or vaginal probiotics compared to a placebo group. While more large-scale studies are needed, the existing evidence points to a potential, low-risk way to be proactive about your microbiome health.
A Specific Probiotic Routine: Strains, Dosage, and Timing
If you’re considering adding probiotics to your routine, it’s not as simple as grabbing any bottle off the shelf. The research points to very specific strains that have been studied for their impact on vaginal health and GBS. Think of it like getting a specific dog for a specific job; you wouldn’t get a chihuahua to herd sheep. The same is true for probiotics.
Key Probiotic Strains for GBS Support
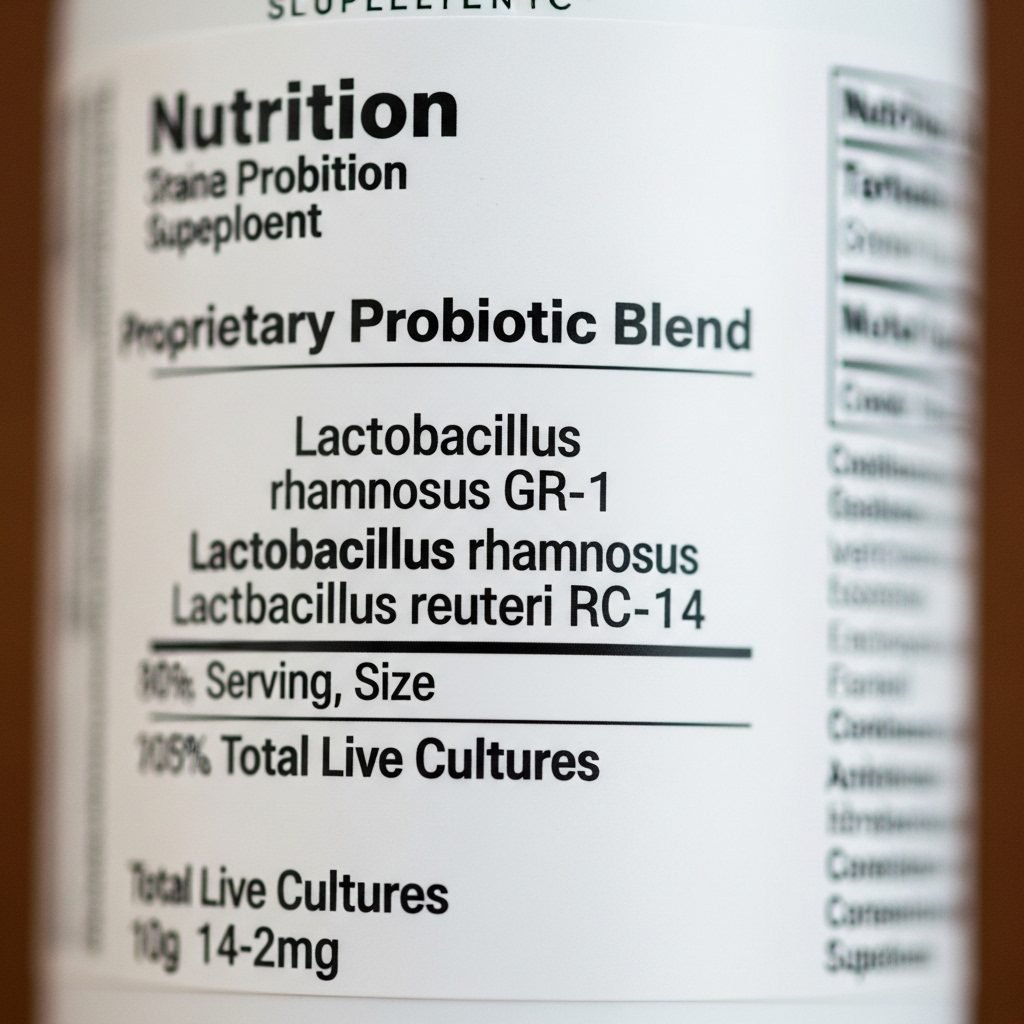
The most-studied strains for vaginal health and their potential to combat GBS colonization belong to the Lactobacillus genus. Look for supplements that specifically list these strains:
- Lactobacillus rhamnosus (especially strain GR-1): This is one of the most well-researched strains for urogenital health. It has been shown to adhere to vaginal cells and inhibit the growth of pathogens.
- Lactobacillus reuteri (especially strain RC-14): Often paired with GR-1, this strain helps produce compounds that are antimicrobial and can help restore a healthy balance.
- Lactobacillus crispatus: This is a cornerstone species of a healthy vaginal microbiome. High levels of L. crispatus are strongly associated with vaginal health and a lower incidence of bacterial vaginosis and other imbalances.
- Other supportive strains: Lactobacillus gasseri and Lactobacillus jensenii are also frequently found in a healthy vaginal flora.
Dosage, CFUs, and Timing
When looking at a supplement label, you’ll see a number followed by “CFU,” which stands for Colony-Forming Units. This indicates the number of viable bacteria in each dose. For GBS support, most studies use dosages ranging from 2 to 10 billion CFUs per day. It’s generally best to start in your third trimester, as soon as you get your diagnosis, or even proactively before your GBS test. Continue taking it through the remainder of your pregnancy and into the postpartum period to help support your microbiome’s recovery after birth and potential antibiotic exposure.
Here is a breakdown of key strains and their roles:
| Probiotic Strain | Potential Role in GBS Support | Common Food Sources |
|---|---|---|
| Lactobacillus rhamnosus GR-1 | Inhibits GBS growth and adherence to vaginal lining. | Primarily found in supplements; some yogurts and kefirs. |
| Lactobacillus reuteri RC-14 | Produces antimicrobial substances; works synergistically with GR-1. | Found in some dairy products and fermented foods; most potent in supplements. |
| Lactobacillus crispatus | A key indicator of overall vaginal health; produces high levels of lactic acid. | Very rare in foods; best obtained through targeted supplements. |
Always choose a reputable brand that guarantees CFU count through the expiration date and, if possible, is third-party tested. Discuss the specific brand and dosage with your midwife, OB-GYN, or a naturopathic doctor before starting any new supplement.
Conclusion
Navigating a GBS-positive diagnosis is about layering your care. Your primary layer of protection for your baby is the proven, effective protocol of IV antibiotics during labor. This is your safety net, and it’s a very strong one. Think of a proactive probiotic routine and a microbiome-friendly diet as an additional, supportive layer. You are not replacing medical advice; you are complementing it by nurturing your body’s own ecosystem.
You are your baby’s best advocate. Asking questions, doing research, and exploring supportive measures like probiotics is a sign of your deep love and commitment. Have an open conversation with your provider about everything you’ve learned. Together, you can create a plan that makes you feel safe, informed, and empowered as you prepare to meet your little one.
Medical Disclaimer
The information provided in this article is for educational and informational purposes only and is not intended as medical advice. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.