Severe Morning Sickness? 7 Survival Items For When Ginger Just Won’t Cut It
If one more person tells you to “just try some ginger ale and crackers,” you might scream. You’re not just feeling a little queasy in the morning; you’re experiencing a level of nausea and vomiting that is completely debilitating. It’s isolating, exhausting, and frankly, terrifying. As a doula and maternal health educator, I want to start by saying: I see you, and what you are experiencing is real and valid.
Severe morning sickness, and its most extreme form, Hyperemesis Gravidarum (HG), is not a psychological issue or an overreaction. It is a legitimate medical condition that requires a serious, multi-faceted approach to management. The well-meaning but simplistic advice often fails because it doesn’t address the severity of the condition. This article is for you—the expectant parent who is past the point of ginger tea. We will explore the critical difference between typical and severe nausea, discuss when to call your provider, and detail seven tangible survival items and strategies that can help you navigate this incredibly challenging time.
Understanding the Spectrum: When ‘Morning Sickness’ Becomes Severe
Understanding the Spectrum: When ‘Morning Sickness’ Becomes Severe
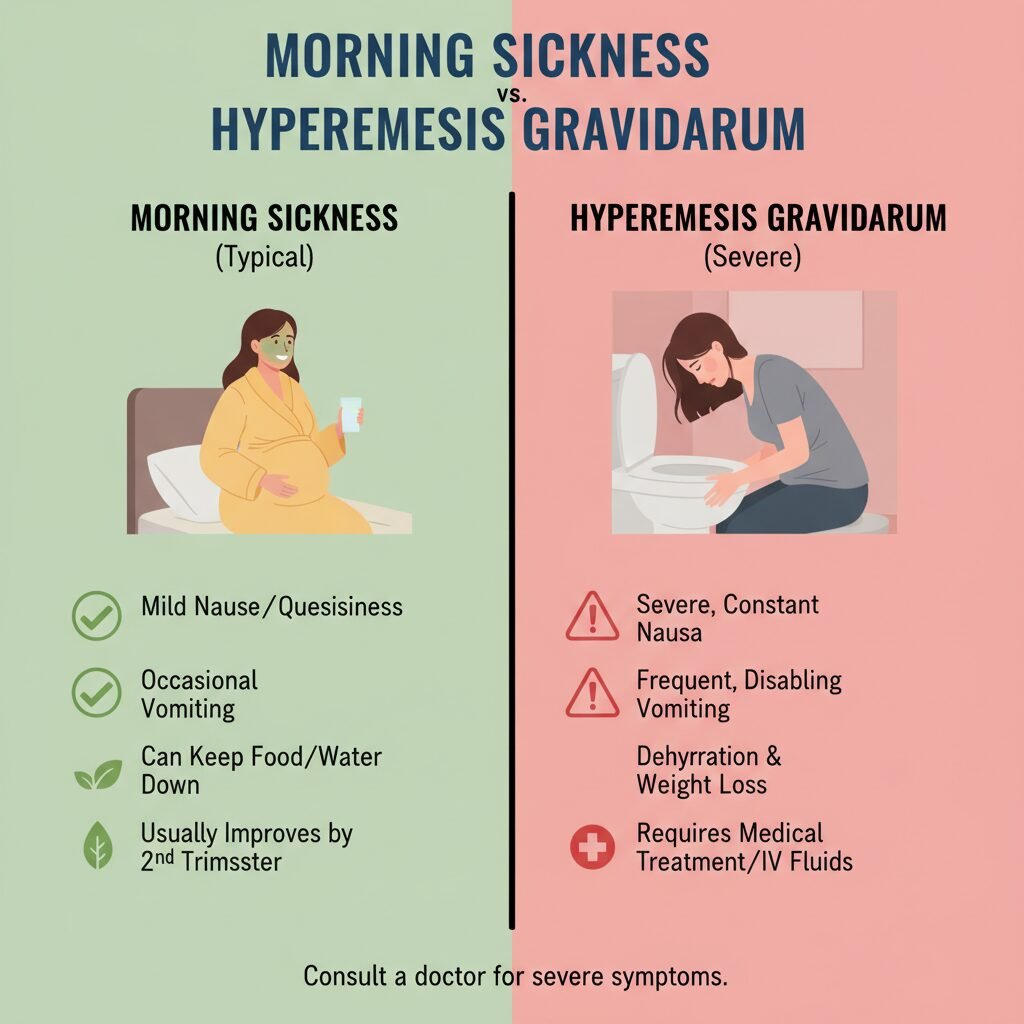
The term ‘morning sickness’ is a profound misnomer. For many, it’s all-day-and-all-night sickness. For most pregnant people (around 70-80%), this involves waves of nausea and occasional vomiting, primarily in the first trimester. It’s unpleasant, but generally manageable. However, for a smaller percentage, the experience is vastly different. It’s crucial to distinguish between typical Nausea and Vomiting of Pregnancy (NVP) and a more severe condition like Hyperemesis Gravidarum (HG).
HG is a diagnosis characterized by persistent, severe nausea and vomiting that leads to significant weight loss (more than 5% of pre-pregnancy weight), dehydration, and electrolyte imbalances. It can require hospitalization for IV fluids and nutritional support. Understanding where you fall on this spectrum is the first step toward getting the right help.
Key Differences: NVP vs. Severe NVP/HG
| Symptom/Factor | Typical Morning Sickness (NVP) | Severe Morning Sickness / Hyperemesis Gravidarum (HG) |
|---|---|---|
| Frequency of Vomiting | Occasional, perhaps 1-2 times per day. Does not prevent hydration or some food intake. | Persistent, often multiple times per day. Prevents keeping down most food and liquids. |
| Hydration Status | Able to stay hydrated, even if it’s a challenge. Urine is light yellow. | Signs of dehydration are present: dark urine, infrequent urination, dizziness, dry mouth. |
| Weight Change | Minimal to no weight loss. May gain weight slowly. | Weight loss of 5% or more of pre-pregnancy body weight. |
| Nutritional Intake | Able to eat some foods at some point during the day. | Inability to tolerate smells, sights, or even thoughts of food. Severe food aversions. |
| Daily Functioning | Functioning is impaired, but daily tasks are usually possible. | Unable to work or care for family. Often bedridden and completely debilitated. |
| Medical Intervention | Usually managed with diet and lifestyle changes. | Often requires medical intervention, including IV fluids and prescription medication. |
Recognizing these differences is not about creating fear; it’s about empowerment. Knowing these signs helps you advocate for yourself effectively with your healthcare provider.
The Foundational First Step: When to Call Your Doctor or Midwife

The Foundational First Step: When to Call Your Doctor or Midwife
Before you try any new product or strategy, the most critical step is communication with your healthcare provider. Self-advocacy is paramount when you are this sick. You are the expert on your body, and if you feel something is seriously wrong, you need to be heard. Do not let anyone, including medical professionals, dismiss your symptoms as “normal pregnancy discomforts.”
Red Flag Symptoms Warranting an Immediate Call:
- You have not been able to keep any liquids down for more than 8-12 hours.
- You are vomiting blood or a substance that looks like coffee grounds.
- You are experiencing signs of severe dehydration: dizziness when standing, confusion, extreme fatigue, a racing heart, or not urinating for more than 8 hours.
- You have lost more than 2 pounds in a single week.
- You are experiencing abdominal pain, fever, or headache alongside the vomiting.
When you call, be prepared to be specific. Tell them exactly how many times you have vomited, what you’ve tried to eat or drink, your last urination, and your current weight compared to your pre-pregnancy weight. This data helps them understand the severity and determine the next steps, which could range from a simple office visit to recommending you go to the hospital for IV rehydration and to rule out other issues.
This is not the time to be stoic. Your health and your baby’s health depend on adequate hydration and nutrition. Seeking medical help is a sign of strength and responsible parenting.
Survival Item #1 & #2: Advanced Hydration & Acupressure Bands

Survival Item #1 & #2: Advanced Hydration & Acupressure Bands
1. Advanced Hydration Tools
When you can’t keep water down, the risk of dehydration escalates quickly. This is where you need to think beyond a simple glass of water. The goal is to get any fluids in, in any form possible. Often, very cold or frozen liquids are more tolerable.
- Electrolyte Replacement: Dehydration isn’t just a loss of water; it’s a loss of essential salts and minerals. Sip on pregnancy-safe electrolyte drinks or powders mixed with the small amount of water you can tolerate. Coconut water is another natural option.
- Ice Chips & Popsicles: Sometimes, the act of drinking is what triggers vomiting. Sucking on ice chips or sugar-free popsicles provides slow, steady hydration that can bypass that trigger.
- The Syringe Method: It may sound extreme, but for some with HG, using a child’s medicine syringe to slowly squirt 5ml of an electrolyte drink into the cheek every 10-15 minutes is the only way to get fluids in.
2. Acupressure Bands
Acupressure is a non-invasive, drug-free option that provides relief for many. Brands like Sea-Band work by applying continuous pressure to the P6 (Nei-Kuan) acupressure point on the inner wrist. This point is believed to relieve nausea.
For these to be effective, placement is key. The plastic stud should press on the P6 point, which is located about three finger-widths down from the first wrist crease, directly between the two central tendons. While not a cure-all, many find they take the “edge” off the nausea, making it slightly more bearable and sometimes preventing a wave of nausea from escalating into vomiting. They can be worn 24/7 and are a safe first line of defense or a complementary therapy alongside medical treatments.
Survival Item #3 & #4: The Vitamin B6/Doxylamine Combo & The ‘BRATT’ Diet Evolved

Survival Item #3 & #4: The Vitamin B6/Doxylamine Combo & The ‘BRATT’ Diet Evolved
3. Vitamin B6 and Doxylamine (Unisom)
Disclaimer: Always consult your healthcare provider before starting any new medication or supplement during pregnancy.
This over-the-counter combination is often the first-line pharmacological treatment recommended by OB-GYNs and midwives for NVP. The American College of Obstetricians and Gynecologists (ACOG) supports its use as a safe and effective option. The combination is sold as a prescription drug called Diclegis, but your provider may recommend you purchase the components separately.
- How it works: Vitamin B6 (pyridoxine) has been shown to reduce nausea, though the exact mechanism isn’t fully understood. Doxylamine succinate (found in Unisom SleepTabs) is an antihistamine that has anti-nausea properties and can cause drowsiness, which can be a welcome side effect when you’re miserable and sleep-deprived.
- Typical Dosing: A common regimen is to take Vitamin B6 throughout the day and a half or whole tablet of Unisom at night. Again, you must get the correct dosage and schedule from your provider.
4. The ‘BRATT’ Diet Evolved
The old advice was the BRAT diet: Bananas, Rice, Applesauce, Toast. We can evolve this. The key is bland, simple, and often cold foods that don’t have strong odors.
- Bland Carbohydrates: Plain baked potatoes, saltine crackers, dry cereal, plain pasta, and pretzels can be stomach-settling. Keep them by your bed and eat a few before you even sit up in the morning to help stabilize blood sugar.
- The Power of Cold: Cold foods have significantly less smell than hot foods. A strong smell can be a powerful nausea trigger. Try cold applesauce, yogurt, cottage cheese, or a simple fruit smoothie (if you can tolerate it).
- Think Small and Frequent: An empty stomach often leads to more intense nausea. Aim to eat a tiny amount—even just two crackers or a spoonful of yogurt—every 1 to 2 hours. This prevents your stomach from becoming completely empty and keeps blood sugar levels more stable.
Survival Item #5 & #6: Protein Power & Sensory Management Tools

Survival Item #5 & #6: Protein Power & Sensory Management Tools
5. Protein Power
While carbohydrates are often easier to stomach initially, a lack of protein can exacerbate the nausea cycle. Protein helps to stabilize blood sugar for longer periods than simple carbs. The challenge is finding tolerable sources.
- Protein Shakes/Powders: A simple, cold protein shake can be a lifesaver. Look for unflavored or mildly flavored (like vanilla) powders that are third-party tested and free from questionable additives. Mix with water, milk, or a milk alternative. Sipping one slowly over an hour can be easier than eating a solid meal.
- Simple, Solid Proteins: If you can manage solids, think small and simple. A cheese stick, a hard-boiled egg (if the smell is tolerable), a handful of almonds, or a spoonful of peanut butter on a cracker can provide that crucial protein boost.
- Bone Broth: Warm, salty bone broth can be incredibly soothing and provides protein, collagen, and electrolytes. Sip it from a mug like tea.
6. Sensory Management Tools
During pregnancy, your senses are often in overdrive, especially your sense of smell (hyperosmia). A scent that was once pleasant can become a powerful nausea trigger. Creating a sensory-neutral environment is a key survival strategy.
- Unscented Everything: Switch to unscented soap, deodorant, lotion, and laundry detergent. Ask your partner and other household members to do the same. This can dramatically reduce triggers.
- Odor Control: Keep a cut lemon or a small dish of coffee grounds nearby to sniff when a bad smell arises; these can ‘reset’ your sense of smell. An air purifier can also help remove lingering odors from the home.
- Light and Sound Blockers: Sometimes, the world is just too much. Blackout curtains, a comfortable eye mask, and noise-canceling headphones or earplugs can help you create a dark, quiet ‘cave’ where you can rest without overstimulation, which often makes nausea worse.
Survival Item #7: A Robust Emotional Support System

Survival Item #7: A Robust Emotional Support System
This may be the most important item on the list. The physical toll of severe morning sickness is immense, but the mental and emotional toll is often overlooked. It is profoundly isolating to be this sick. You may feel like you are failing at pregnancy, or experience anxiety and depression. You are not failing. You are surviving a serious medical condition.
Building Your Village:
- Communicate with Your Partner: Be explicit about what you need. Your partner may feel helpless and unsure of how to support you. Give them concrete tasks: ‘Can you please handle all the cooking? The smells are making me sick.’ or ‘I need you to be the gatekeeper and explain to family why we can’t have visitors.’
- Find Your People Online: Connecting with others who understand is invaluable. Organizations like the HER Foundation offer resources, research, and online support groups filled with people who have been through it. Reading their stories and sharing your own can be a lifeline.
- Seek Professional Mental Health Support: There is no shame in needing help. A therapist, particularly one who specializes in perinatal mental health, can provide you with coping strategies and a safe space to process the trauma and anxiety associated with HG.
Remember, accepting help is not a weakness. Delegating tasks, asking for support, and prioritizing your well-being is not just good for you; it’s essential for your growing baby. You need to put on your own oxygen mask first. Allow your village to care for you during this intense season.
Conclusion
You Are a Warrior
Navigating severe morning sickness or Hyperemesis Gravidarum is one of the toughest challenges a person can face during pregnancy. It tests you physically, mentally, and emotionally. The journey is not about finding a single magic cure, but about building a personalized toolkit of survival strategies. From advanced hydration and medical support to sensory management and leaning on your village, each small action contributes to your overall ability to cope.
Please remember to be kind to yourself. You are growing a human being under extreme duress. That is nothing short of heroic. Keep advocating for your needs, accept help when it’s offered, and hold on to the knowledge that this is temporary. It will not last forever, and on the other side of this is the incredible reward of meeting your child. You are strong, you are capable, and you will get through this.
Medical Disclaimer
The information provided in this article is for educational and informational purposes only and is not intended as medical advice. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.