Just Swollen Ankles or Danger? 5 Silent Signs of Preeclampsia You Can’t Ignore
Pregnancy is a journey filled with new sensations, and let’s be honest, a lot of them are…uncomfortable. Swollen feet and ankles, or edema, are so common that they’ve become a hallmark of the third trimester. You might find yourself swapping stylish shoes for supportive slippers and laughing it off as just another part of the process. And most of the time, you’d be right. But as a doula and maternal health educator, I’m here to gently guide you through a crucial distinction: the difference between normal pregnancy swelling and a potential red flag for a serious condition called preeclampsia.
It’s a word that can bring a wave of anxiety, and that’s completely understandable. The fear of the unknown is powerful, especially when you’re responsible for the tiny life growing inside you. Our goal here isn’t to cause alarm, but to replace that fear with knowledge. This article will empower you to listen to your body’s whispers before they become screams. We’ll walk through the five often-overlooked, silent signs of preeclampsia that go beyond swollen ankles, so you can feel confident in knowing when to rest your feet and when it’s time to call your doctor or midwife. You are your own best advocate, and we’re here to help you use your voice.
Understanding Preeclampsia: More Than Just High Blood Pressure
Before we dive into the symptoms, let’s clarify what preeclampsia actually is. At its core, preeclampsia is a pregnancy-specific condition characterized by high blood pressure and signs of damage to another organ system, most often the liver and kidneys. It typically develops after 20 weeks of gestation in women whose blood pressure had previously been normal.
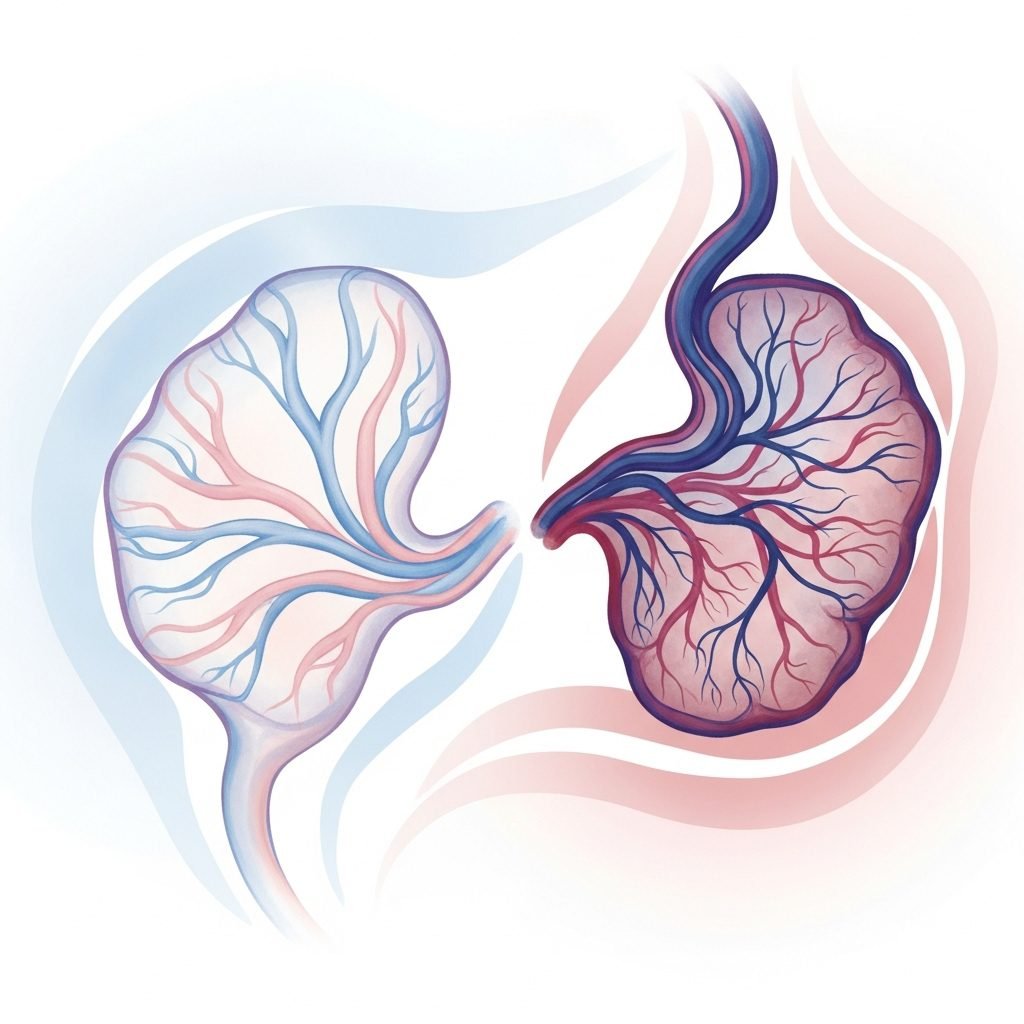
Think of your placenta as the intricate life-support system for your baby, delivering oxygen and nutrients through a complex network of blood vessels. In a healthy pregnancy, these vessels develop to handle increased blood flow. With preeclampsia, these blood vessels don’t develop or function properly. They are narrower than normal and react differently to hormonal signaling, which can lead to restricted blood flow to the placenta and a rise in the mother’s blood pressure.
Why It’s So Critical to Monitor
Left untreated, preeclampsia can lead to serious—even fatal—complications for both mother and baby. For the mother, it can cause organ damage (liver, kidneys, brain), seizures (a condition called eclampsia), and stroke. For the baby, restricted blood flow to the placenta can mean less oxygen and nutrients, leading to slow growth (intrauterine growth restriction), low birth weight, preterm birth, and in severe cases, stillbirth.
Knowing the signs isn’t about creating fear; it’s about fostering awareness. Your body communicates with you constantly during pregnancy. Learning its language is one of the most powerful things you can do for yourself and your baby.
The challenge with preeclampsia is that its onset can be gradual or sudden, and some of its earliest signs can easily be mistaken for normal pregnancy discomforts. That’s why we call them ‘silent’ signs—they don’t always announce themselves loudly. This is precisely why your regular prenatal check-ups, where your provider monitors your blood pressure and urine protein levels, are so vitally important.
The 5 Silent Signs: Listening to Your Body’s Whispers

Beyond the numbers on a blood pressure cuff, your body offers clues. It’s time to tune in and learn to recognize the signals that warrant a conversation with your healthcare provider. These are the symptoms that you might be tempted to dismiss, but absolutely shouldn’t.
1. Severe or Persistent Headaches
We all get headaches. But a preeclampsia headache is different. It’s often described as a severe, throbbing pain, sometimes like a migraine, that doesn’t go away with rest, hydration, or typical over-the-counter pain relievers like acetaminophen (Tylenol). If you have a headache that feels unusually intense or just won’t quit, it’s a significant sign that needs to be reported.
2. Vision Changes
This is one of the most specific and concerning signs. Don’t brush off changes to your eyesight as simple fatigue. Preeclampsia can affect your central nervous system and cause swelling in the brain, which can manifest in your vision. Pay attention to:
- Blurriness or double vision
- Seeing flashing lights, auras, or spots (floaters)
- Sudden sensitivity to light (photophobia)
- Temporary loss of vision
These symptoms are never normal in pregnancy and require an immediate call to your doctor or midwife.
3. Pain in the Upper Abdomen
This is perhaps the most misleading symptom because it’s easily confused with heartburn, indigestion, or gallbladder pain. The key difference is the location and nature of the pain. Preeclampsia-related abdominal pain is usually felt on the right side, just under your rib cage. This is due to liver inflammation. It might feel like a deep, constant ache or a sharp, stabbing pain. If you’re experiencing this kind of localized pain that isn’t relieved by antacids, it’s a critical warning sign.
4. Sudden or Severe Swelling (Edema)
Yes, we’re back to swelling, but with important distinctions. Gradual swelling in your feet and ankles that is worse at the end of the day and improves with rest is typically normal. The swelling associated with preeclampsia is different:
- It’s sudden: Your rings suddenly don’t fit, or your face looks puffy overnight.
- It’s widespread: You notice significant swelling not just in your feet and legs, but also in your hands and face.
- It causes ‘pitting’: If you press your thumb firmly into the swollen skin for a few seconds, an indentation remains after you release the pressure. This is called pitting edema and indicates significant fluid retention.
5. Rapid Weight Gain
Gaining weight is an expected part of pregnancy, but the pace matters. A sudden jump on the scale—gaining more than two or three pounds in a single week—is not usually related to the baby’s growth or normal fat storage. It’s almost always due to fluid retention, a direct result of the kidney changes that can occur with preeclampsia. While your weight can fluctuate, a rapid and sustained increase is a red flag that your body is holding onto too much fluid.
Who Is at Risk? Understanding Your Personal Factors

While any pregnant person can develop preeclampsia, some factors can increase your risk. Knowing if you fall into a higher-risk category doesn’t guarantee you’ll develop the condition, but it does mean that you and your provider should be extra vigilant. It’s about proactive care, not panic.
Common risk factors include:
- First-time pregnancy: Preeclampsia is more common during a person’s first pregnancy.
- A personal or family history of preeclampsia: If you’ve had it before, or if your mother or sister had it, your risk is higher.
- Carrying multiples: Being pregnant with twins, triplets, or more increases the strain on your body and placenta.
- Pre-existing medical conditions: Chronic high blood pressure, kidney disease, diabetes, and autoimmune conditions like lupus can increase your risk.
- Age: Pregnancies at either end of the spectrum (very young teens or those over 40) carry a higher risk.
- Obesity: A higher pre-pregnancy BMI is a known risk factor.
- In vitro fertilization (IVF): Some studies suggest a slightly increased risk for pregnancies conceived via IVF.
If you have any of these risk factors, your doctor may recommend more frequent monitoring or suggest preventative measures, such as taking a low-dose aspirin daily starting late in the first trimester. This is a decision to be made only in consultation with your healthcare provider. Having an open dialogue about your personal and family health history from your very first prenatal appointment is a key step in proactive care.
Your Personal Symptom Tracker: An At-Home Guide
Feeling empowered often comes from having tangible information. If you have risk factors or are simply feeling anxious, tracking your symptoms can provide peace of mind and create a clear, objective record to share with your provider. It helps you move from a vague feeling of ‘something is off’ to specific data points. Consider using a simple chart like the one below in a notebook or on your phone. If your provider has recommended at-home blood pressure monitoring, be sure to include those readings.
This is not a tool for self-diagnosis. It is a tool for communication and self-advocacy. It helps you have a more productive conversation with your care team, grounded in specific observations.
| Date | Time | Blood Pressure (if monitoring) | Swelling (Scale 1-5) | Headache/Vision Issues? | Notes (e.g., upper belly pain, feeling ‘off’) |
|---|---|---|---|---|---|
| Example: 10/26 | 8:00 AM | 135/85 | 3 (hands & feet) | Yes, dull headache | Felt a bit dizzy after standing up. |
| Example: 10/26 | 6:00 PM | 142/90 | 4 (face feels puffy) | Headache is worse | Called the on-call midwife to report symptoms. |
Conclusion
Navigating the physical and emotional landscape of pregnancy is a profound experience. It’s a time of joy, anticipation, and, yes, a little bit of worry. Your body is doing something truly miraculous, and it’s okay to be hyper-aware of every new ache and pain. The most important takeaway from this article is to trust your intuition. You know your body better than anyone else. If something feels wrong, it is always, always worth a phone call to your doctor or midwife.
Never dismiss your concerns as ‘just being paranoid’ or ‘not wanting to be a bother.’ Your healthcare team is there to support you, and they would much rather hear from you a dozen times about something that turns out to be nothing than miss the one call that truly matters. Recognizing the silent signs of preeclampsia isn’t about adding another worry to your plate; it’s about giving you the tools to be an active, empowered participant in your own care. You are strong, you are capable, and by staying informed, you are giving both yourself and your baby the best possible protection.
Medical Disclaimer: The information provided in this article is for educational and informational purposes only and is not intended as medical advice. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.