Won’t Stop Bleeding? The Truth About Pregnancy Nosebleeds And How To Stop Them
The sudden, unexpected sight of blood during pregnancy can send a wave of panic through any expectant parent. When it comes from your nose, it can be both confusing and frightening. You might find yourself asking, ‘Is this normal? Is the baby okay? Why is this happening?’ First, take a deep breath. Pregnancy nosebleeds, medically known as epistaxis, are an incredibly common and usually harmless side effect of the amazing changes your body is undergoing. You are not alone in this experience.
The surge in hormones and blood volume required to grow a healthy baby can put extra pressure on the tiny, delicate blood vessels in your nasal passages, making them more prone to rupture. While startling, most cases are minor and can be managed easily at home. This comprehensive guide, written from a doula and maternal health perspective, will walk you through the science behind pregnancy nosebleeds, provide a clear, step-by-step plan to stop them effectively, offer preventative strategies, and, most importantly, help you understand the specific signs that mean it’s time to contact your healthcare provider. Our goal is to replace your anxiety with confidence and empower you with the knowledge to navigate this common pregnancy symptom safely.
Why Pregnancy Can Cause Unexpected Nosebleeds
Understanding the Physiological Changes
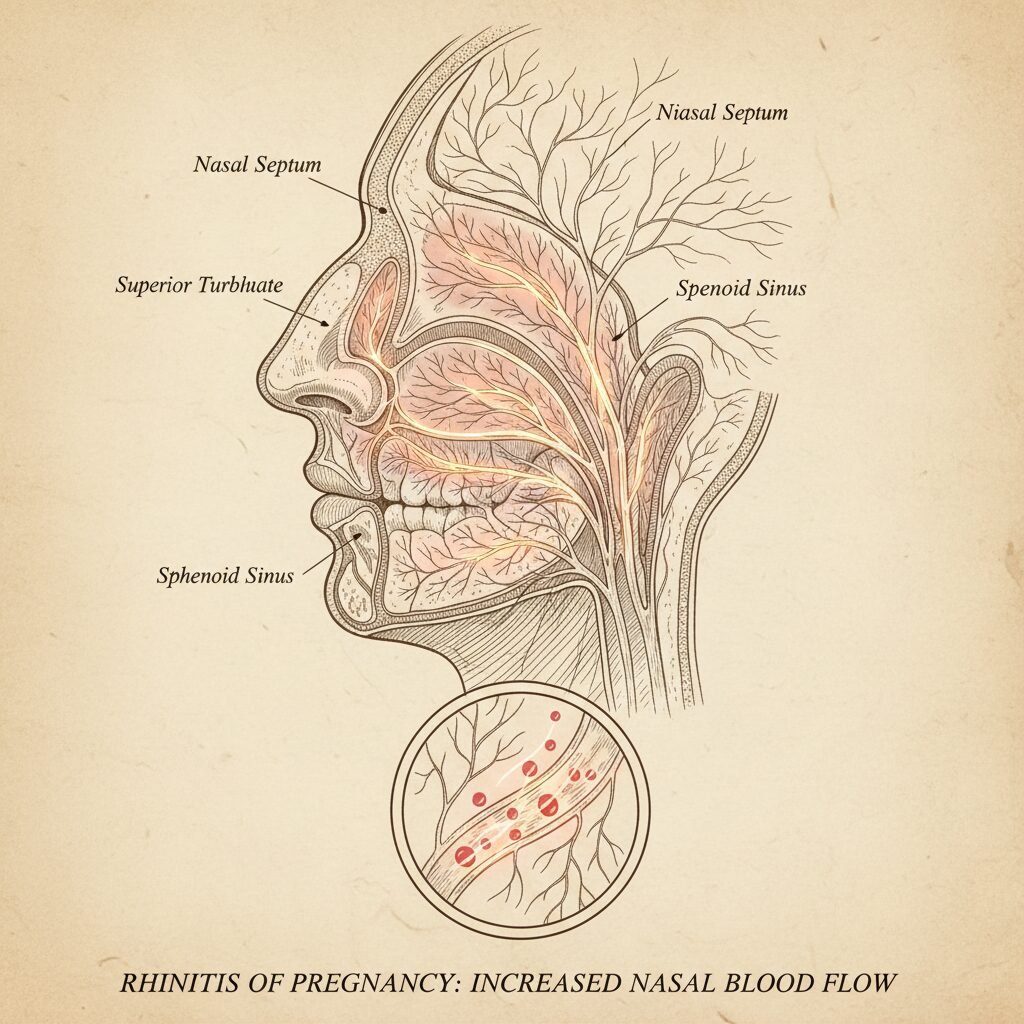
To understand why your nose might suddenly start bleeding, it’s helpful to appreciate the profound vascular changes happening throughout your body. From the moment of conception, your system ramps up production of hormones like estrogen and progesterone. These hormones are essential for sustaining the pregnancy, but they also have wide-ranging effects, including increasing blood flow to all of your mucous membranes—the moist tissues lining your nose, mouth, and other cavities.
The Role of Increased Blood Volume
One of the most dramatic changes during pregnancy is the expansion of your blood volume. By the third trimester, you may have up to 50% more blood circulating to support the placenta and your baby’s development. This increased volume places additional pressure on your entire circulatory system, including the network of tiny capillaries in your nose. These vessels are already close to the surface, and the added pressure makes them swell and become more fragile, leading to a higher likelihood of a rupture from something as simple as a sneeze, blowing your nose, or even just dry air.
Hormonal Influence on Blood Vessels
Estrogen is known to cause blood vessels to dilate (widen), while progesterone relaxes their walls. This combination makes the vessels in your nasal lining, known as Kiesselbach’s plexus, particularly susceptible. Think of it like a network of small, delicate garden hoses that suddenly have significantly more water pressure flowing through them. It doesn’t take much for a small leak to spring.
Contributing Environmental Factors
While internal changes are the primary cause, external factors can certainly exacerbate the issue:
- Dry Air: Arid climates, centrally heated homes in winter, or air conditioning in summer can dry out your nasal passages, making the tissue brittle and more likely to crack and bleed.
- Colds and Allergies: Inflammation from a cold, sinus infection, or seasonal allergies can irritate the lining of your nose. Frequent blowing or wiping can also trigger a bleed.
- Minor Trauma: Even gentle nose-blowing or rubbing can be enough to break a fragile vessel.
Recognizing that these physiological changes are a normal part of a healthy pregnancy is the first step in managing the anxiety that nosebleeds can cause. Your body is simply adapting to the incredible task of growing a new life.
A Step-by-Step Guide: How to Safely Stop a Pregnancy Nosebleed
Immediate and Effective First Aid
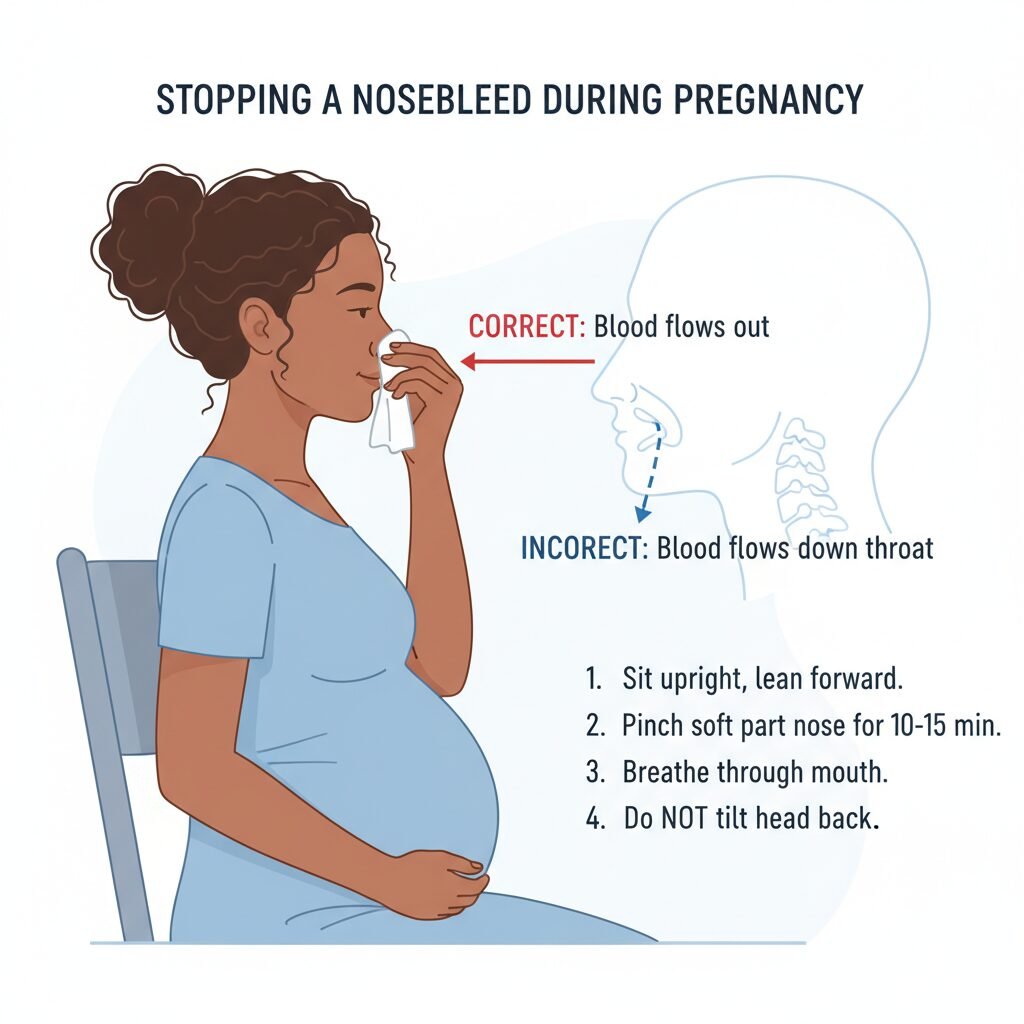
When a nosebleed starts, your first instinct might be to tilt your head back. This is a common myth and can actually cause problems, as it allows blood to run down your throat, which can lead to nausea, vomiting, or even aspiration. Instead, follow these safe and effective steps to manage the bleeding calmly.
- Stay Calm and Sit Upright: Panic can increase your heart rate and blood pressure, potentially making the bleeding worse. Sit down in a comfortable chair. Keeping your head above the level of your heart is important.
- Lean Slightly Forward: This is the most critical step. Lean your body forward from the waist. This ensures that the blood drains out of your nose rather than down the back of your throat. Use a tissue or a towel to catch the blood.
- Pinch Your Nose Correctly: Using your thumb and index finger, firmly pinch the soft, fleshy part of your nose, just below the bony bridge. You need to press the bleeding vessel against the central cartilage (septum) to stop the flow. Squeezing the hard, bony part will have no effect.
- Apply Consistent Pressure: Hold this pressure continuously for at least 10 to 15 minutes. Resist the urge to release the pressure to check if the bleeding has stopped. It takes time for a proper clot to form. Use a clock to time yourself. While you wait, focus on breathing slowly and calmly through your mouth.
- Use a Cold Compress: While pinching your nose, you can apply a cold pack, a bag of frozen vegetables wrapped in a towel, or a cold cloth to the bridge of your nose and your cheeks. The cold helps to constrict the blood vessels, which can slow the bleeding and aid in clotting.
What to Do After the Bleeding Stops
Once the bleeding has ceased, it’s important to protect the newly formed clot. For the next several hours, and ideally for the rest of the day, avoid the following:
- Blowing your nose: This can easily dislodge the clot and restart the bleeding. If you must sneeze, do so with your mouth open to reduce pressure in the nasal passages.
- Strenuous activity: Avoid heavy lifting, exercise, or any activity that raises your blood pressure.
- Bending over: Try to keep your head above your heart. When you need to pick something up, bend at your knees, not your waist.
- Hot drinks or hot showers: The heat and steam can dilate the blood vessels again, potentially triggering another bleed.
Remember, patience is key. Allowing the clot to fully stabilize is crucial for preventing a recurrence.
Proactive Measures: Can I Prevent Pregnancy Nosebleeds?

Creating a Nose-Friendly Environment
While you can’t change the hormonal and circulatory shifts of pregnancy, you can take several proactive steps to minimize the frequency and severity of nosebleeds. The goal is to keep your nasal passages moist and avoid irritation.
Hydration and Humidification
- Stay Well-Hydrated: Drinking plenty of water throughout the day is one of the best ways to keep all your mucous membranes, including those in your nose, well-hydrated from the inside out. Aim for 8-12 glasses of water daily.
- Use a Humidifier: Running a cool-mist humidifier in your bedroom at night can make a significant difference, especially during dry winter months or if you live in an arid climate. It adds moisture to the air you breathe, preventing your nasal lining from drying out.
Topical Solutions and Gentle Habits
- Saline Nasal Spray: A simple, over-the-counter saline (saltwater) spray is perfectly safe during pregnancy and can be used several times a day to moisten your nasal passages. It helps to clear irritants and prevent cracking.
- A Dab of Ointment: Gently applying a small amount of a water-based lubricant, petroleum jelly, or a lanolin-based ointment just inside your nostrils with a cotton swab can create a protective barrier. This is especially helpful before bed.
- Blow Your Nose Gently: When you have a cold or allergies, resist the urge to blow your nose forcefully. Press a finger against one nostril and blow gently through the other.
Nutritional Support
Ensuring you have adequate Vitamin C in your diet can help strengthen capillaries and promote healthy connective tissue. Excellent sources include citrus fruits, bell peppers, strawberries, broccoli, and kiwi. While dietary sources are best, always consult your healthcare provider before starting any new supplements during pregnancy.
| Preventative Strategy | Why It Works | How to Implement |
|---|---|---|
| Increase Hydration | Keeps mucous membranes moist from the inside. | Drink 8-12 glasses of water per day. |
| Use a Humidifier | Adds moisture to the air, preventing nasal dryness. | Run a cool-mist humidifier in your bedroom at night. |
| Saline Nasal Spray | Directly moisturizes and soothes nasal passages. | Use 1-2 sprays in each nostril as needed. |
| Gentle Ointment | Creates a protective barrier against dry air. | Apply a small amount inside nostrils with a cotton swab. |
When to Worry: Red Flags and When to Call Your Doctor or Midwife

Knowing When Professional Medical Advice is Necessary
While the vast majority of pregnancy nosebleeds are benign, it is crucial to recognize the signs that may indicate a more serious underlying issue. Your healthcare team is there to support you, and you should never hesitate to reach out if you are concerned. Trust your instincts—if something feels wrong, it is always best to get it checked out.
Seek Immediate Medical Attention or Call Your Provider If:
- The Bleeding is Profuse or Won’t Stop: If you are experiencing heavy, gushing bleeding or if the nosebleed continues for more than 20-30 minutes despite consistently applying direct pressure as described above, it’s time to seek care.
- You Feel Dizzy, Faint, or Weak: These symptoms could indicate significant blood loss and require immediate evaluation.
- The Nosebleed Follows a Head Injury: Any bleeding from the nose after a fall or blow to the head should be assessed by a medical professional right away.
- You Experience Other Concerning Symptoms: A nosebleed accompanied by a severe headache, blurred vision, or seeing spots could be related to high blood pressure or preeclampsia, a serious pregnancy complication. It’s vital to report these symptoms to your doctor or midwife immediately.
- You Have Trouble Breathing: While this is rare, if the bleeding is heavy enough to interfere with your ability to breathe, seek emergency care.
- The Nosebleeds are Chronic and Frequent: If you are having multiple, severe nosebleeds every week, it’s worth discussing with your provider. They may want to rule out other conditions or check your iron levels for anemia.
A Note for Dads and Partners: Your role is vital. Stay calm, help time the 15 minutes of pressure, get a cold compress, and be the one to make the call to the doctor if needed. Your steady support is invaluable.
Your doctor or midwife can assess the situation, check your blood pressure, and provide further guidance. In rare cases, they may need to cauterize the vessel or pack the nose to stop the bleeding. Remember, advocating for your health and the health of your baby is always the right choice.
Conclusion
Navigating the many physical changes of pregnancy can be a journey filled with questions and occasional moments of concern. Pregnancy nosebleeds are a perfect example of a symptom that, while alarming, is most often just another testament to the incredible work your body is doing. By understanding the underlying causes—the surge in hormones and blood volume—you can demystify the experience and reduce your anxiety. Armed with the proper first-aid technique of leaning forward and applying firm, consistent pressure, you can manage most episodes effectively at home.
Furthermore, by taking proactive steps like staying hydrated, using a humidifier, and being gentle with your nose, you can often lessen their frequency. Most importantly, you now know the critical red flags that signal when it’s time to move beyond home care and contact your medical team. Never let fear of ‘bothering’ your doctor or midwife prevent you from seeking reassurance and care. They are your partners on this journey.
Embrace this knowledge as another tool in your parenting toolkit. You are capable, you are informed, and you are doing an amazing job of protecting your health and nurturing the new life within you.
Medical Disclaimer
The information provided in this article is for educational and informational purposes only and is not intended as medical advice. It is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician, midwife, or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.